Surgical procedures
Find out about the different surgical procedures that are sometimes used to treat problems caused by kidney cysts in autosomal dominant polycystic kidney disease (ADPKD).
Contents
- Surgery to treat ADPKD
- Surgery to prepare for haemodialysis
- Surgery to prepare for peritoneal dialysis
- Having one or both kidneys removed
- Having a kidney transplant
- Treating kidney complications
- Minimally invasive procedures
- Cyst surgery
- Having your parathyroid gland removed
- More from the PKD Charity
- More information from others
- Authors and contributors
Surgery to treat ADPKD
Autosomal dominant polycystic kidney disease (ADPKD) is a genetic condition that causes cysts to grow in the kidneys. As these cysts gradually enlarge, kidney function falls, often eventually resulting in kidney failure.
Many aspects of ADPKD can be managed with lifestyle changes and medications. However, some problems that develop in the kidneys – such as pain, infection, bleeding and kidney failure – can mean that surgery is needed. If your treatment team thinks that you could benefit from surgery, they’ll explain why. All the procedures described here are considered safe and outcomes are usually good. But they do have some risks. Your surgeon will talk you through the risks and benefits, what the procedure involves, and any alternatives.
In this fact sheet, we introduce some of the more common surgical procedures that patients with ADPKD can need due to changes in the kidneys. These are:
- Preparation for dialysis
- Having a kidney transplant
- Removing damaged kidneys
- Treating kidney complications
- Treating an overactive parathyroid gland
It’s also possible to need surgery or minimally invasive procedures to treat changes in the liver or a brain aneurysm. You’ll find more information about these treatments in our factsheets on polycystic liver disease and aneurysms.
Surgery to prepare for haemodialysis
Haemodialysis involves passing the blood through a filtering machine, called a dialyser. This removes waste and extra fluid from the blood. If you’re going to start having haemodialysis, you’ll usually first need to have an enlarged blood vessel made under your skin. This is called an arteriovenous fistula (or AV fistula). The fistula is where needles will be inserted into your arm to connect your blood to the dialysis machine.
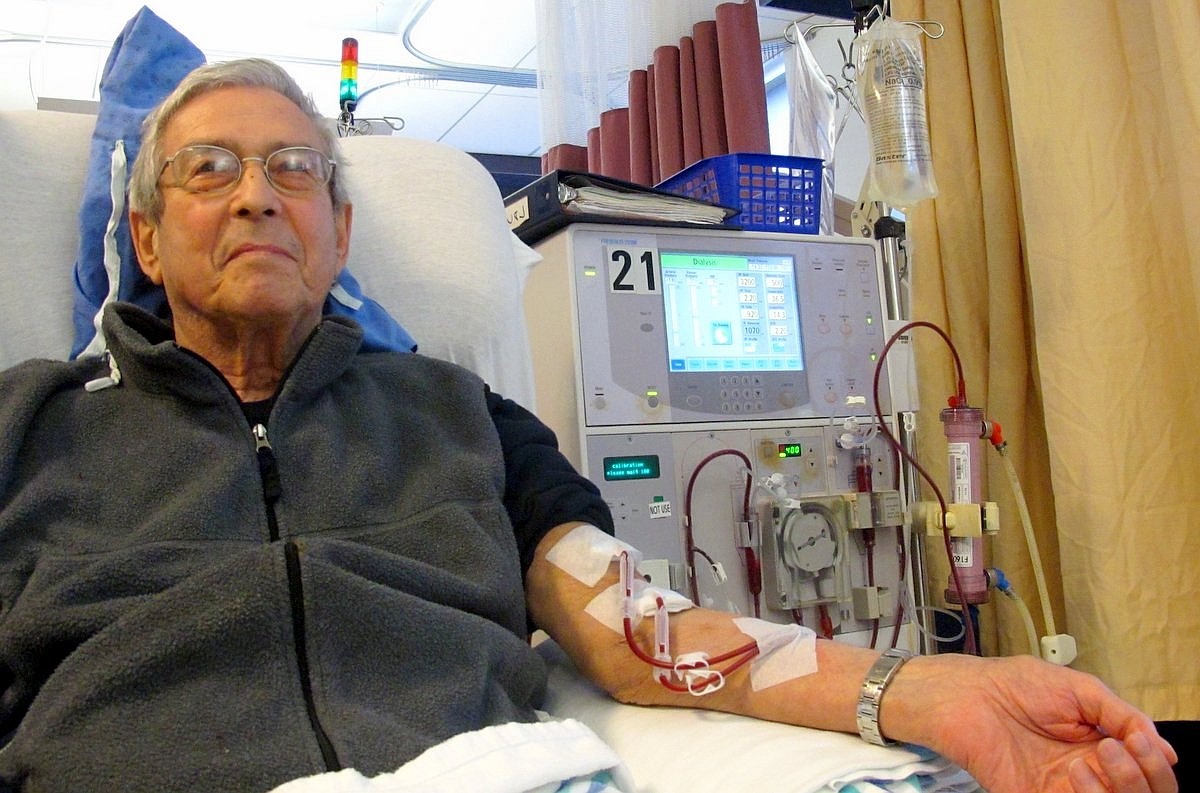
An AV fistula is made by a surgeon by connecting one of your veins (which carries blood to the heart) to one of your arteries (which carries blood away from the heart). AV fistulas help to get good blood flow to the dialyser. Sometimes, a slightly different procedure is used, where an artery is connected to a man-made tube, called a graft.
The procedure is relatively simple and is done under local or general anaesthesia. It is usually done as a ‘day case’, which means you probably won’t need to stay in hospital overnight. The fistula takes about 4 to 8 weeks to heal and become strong. After this time, you’ll be ready for starting haemodialysis.
If you need to start haemodialysis sooner than this, you might have a catheter (tube), placed into a vein in your neck or groin as short-term solution. This is called a central venous catheter. However, these catheters are more likely to get infected, get a blood clot, or cause hardening of the blood vessel than an AV fistula. So, your treatment team will probably recommend an AV fistula if you’ll be having haemodialysis long term.
There is a risk that AV fistulas can get infected. Infections in the blood stream can be serious, so it’s important to keep the area clean
Surgery to prepare for peritoneal dialysis
Peritoneal dialysis uses a special fluid placed in an area of your lower abdomen, known as the peritoneal space. This fluid absorbs toxins. Your peritoneal space houses your bowels and liver and is surrounded by a membrane called the peritoneum.
Before you can start having peritoneal dialysis, you’ll first need simple surgery to have a tube fitted through your skin into your peritoneal space. This tube – called a peritoneal catheter – will stay by your belly button permanently. You’ll use it to add and remove fluid from your abdomen.
The surgery to fit a peritoneal catheter is done under general or local anaesthetic as a day case. It will take 2–3 weeks for the area to heal, and then you can begin having peritoneal dialysis sessions. A downside of peritoneal dialysis is that some people find it hard to get used to having a peritoneal catheter. It’s also possible that bacteria will get into your body via the catheter, which could cause a serious infection. So, it’s important to keep it clean.
Having one or both kidneys removed
If your kidneys begin to fail, your treatment team probably won’t recommend removing them unless they’re causing serious problems. (You can receive a kidney transplant without your own kidneys being disconnected and removed.) Even if your damaged kidneys are no longer filtering waste from your body effectively, they might still be removing excess fluid from your body, and so they can still be useful. Also, having one or both kidneys removed (known as nephrectomy) is a major operation. Like all major operations it has some risks – such as bleeding or getting an infection – and so should only be done when necessary.
However, if your damaged kidneys are causing you a lot of pain and other treatments are not helping, your surgeon may recommend removing them. The pain could be caused by repeated infections or cyst bleeding for example.
Another reason for nephrectomy is if you’re due to have a kidney transplant but your own kidneys are very large and there would not be sufficient room for your new donor kidney. In this instance, one of your own kidneys can be removed to create space.
Nephrectomy is a major operation, so be sure that your surgeon explains the risks and benefits to you. Risks can include:
- bleeding
- problems with the heart or circulation
- injury to other organs, such as bowel, spleen or liver
- infection
- the wound reopening
These might require further treatment or surgery. However, your surgeon will perform the operation extremely carefully to minimise any risk to you.
Your surgeon will talk you through the technique they’ll use to remove your kidney (or kidneys) beforehand. They might need to make a large cut to get to your kidney, but sometimes keyhole surgery (laparoscopy) can be used, which involves a few small cuts being made. Laparoscopy has the advantages of usually being less painful, having a swifter recovery (and so shorter hospital stay) and having less scarring. If your kidneys are very large though, your surgeon will need to make a larger cut to remove them.
If you’re having a kidney removed to make room for a kidney transplant, you’ll probably be ready to have the transplant within 6 to 8 weeks.
A downside of having your kidneys removed is that, unless you have a transplant, you’ll have to be very careful to limit the amount of fluid you drink. This could affect your quality of life.
Having a kidney transplant
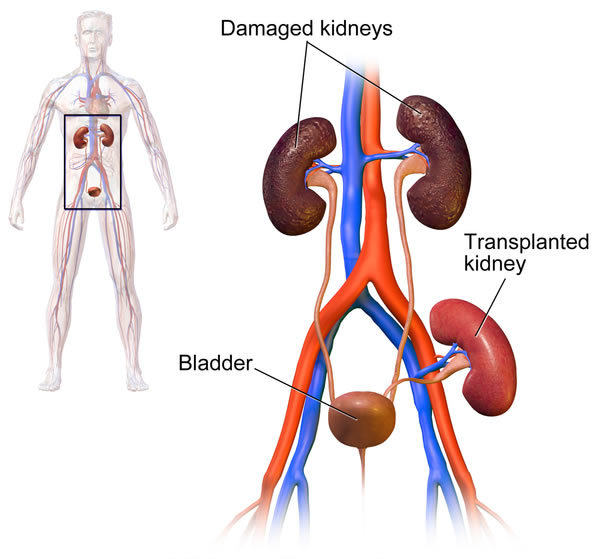
The surgery takes about 3 hours. You’ll need to stay in hospital for about 5 days while you recover. A kidney transplant comes with some risks, including bleeding, internal urine leaks, getting an infection, and having side effects from the drugs you’ll need to take after your operation. We describe these in more detail in our factsheet on kidney transplants.
After your transplant, you’ll be followed up at the transplant clinic by kidney specialists and transplant surgeons to check you’re healthy and that your new kidney is working well.
Treating kidney complications
Complications such as pain from a large cyst or enlarged kidneys might well be treatable without surgery. However sometimes surgery or minimally invasive procedures can be helpful when pain is not improving with pain killers.
Minimally invasive procedures
If you have a large kidney cyst that is causing pain, a specialist radiologist can drain the fluid from it using a large needle. This is called percutaneous cyst aspiration. Your radiologist will use ultrasound or a CT (computed tomography) scan to guide the needle to the cyst.
Unfortunately, cysts usually refill with fluid. Drained cysts can be treated to reduce the chance of them refilling. One way to do this is for the surgeon to inject alcohol into the cyst under local anaesthesia (or general anaesthesia in some cases). This is known as sclerotherapy.
This risk of the procedure depends on how deep the cyst is within the kidney, and also how many cysts you have treated. You may get small amounts of bleeding, some pain or a fever during the procedure, but more serious risks are minimal.
In some countries, other techniques – such as trans-arterial embolisation – are being used in some cases where surgery would be too high risk. For this, the radiologist will give the patient a local anaesthetic and feed a thin tube (a catheter) into one of the arteries in the groin. They’ll feed this tube through the artery into a blood vessel supplying blood into the kidney. They’ll then treat this artery to block it by causing a blood clot to form. This restricts the blood supply to kidney, causing it to shrink. Trans-arterial embolisation might reduce pain and discomfort longer term, although may initially cause pain and fever for a few days. Although this technique is not currently widely used in the UK, it might become useful in some situations in the future.
Cyst surgery
If you have painful cysts, an alternative to sclerotherapy is to remove the part of the wall of the cyst and allow the fluid to drain into the peritoneal space. This process is called deroofing or fenestration. It’s a bigger procedure than sclerotherapy and involves surgery (either keyhole surgery or open surgery) under general anaesthetic. It’s also possible to surgically remove nerves to the kidney so that they no longer feel pain.
These procedures carry the risks associated with surgery, such as bleeding and infection, but work well to reduce pain in most patients.
Having your parathyroid gland removed
If you have kidney failure and are using dialysis, it’s likely that you’ll develop overactive parathyroid glands over time. Your parathyroid glands are four small glands (the size of peas) in your neck that control levels of calcium and phosphate in your body. They’re different to your thyroid gland.
The parathyroid glands can become overactive because kidney failure makes your blood calcium levels fall, and the glands begin to work harder to try to correct this. Overactive parathyroid glands can cause your bones to lose calcium and lead to bone pain. Often, this can be treated with medications. However, if medications don’t work, you may need to have the glands removed surgically. This is called parathyroidectomy.
The operation is done under general anaesthetic and takes about 1 hour. Your surgeon will need to make a cut in your neck to reach the glands. It usually takes a day to recover, meaning you’ll probably need to stay in hospital overnight.
More from the PKD Charity
- Kidney transplantation
- Managing ADPKD pain
- The PKD Charity’s closed UK Facebook Group – many members have had surgical procedures and provide helpful peer support
More information from others
- NHS Choices has information on kidney transplantation and dialysis.
- The National Kidney Federation (www.kidney.org) has information on nephrectomy and hyperparathyroidism – but bear in mind this information is for American patients and NHS practice may differ.
Authors and contributors
Written by Mr Badri Man Shrestha, BSc MBBS MS MPhil MD FRCS(Eng & Gen) Hon.FRCS(Edin) FACS FICS FEBS, Consultant Transplant Surgeon, Sheffield Teaching Hospitals NHS Trust.
Edited by Hannah Bridges, PhD, independent medical writer, HB Health Comms Limited.
With thanks to all those affected by ADPKD who contributed to this publication.
IS Ref No: ADPKD.SP.2017V1.0
UNDER REVIEW
Disclaimer: This information is primarily for people in the UK. We have made every effort to ensure that the information we provide is correct and up to date. However, it is not a substitute for professional medical advice or a medical examination. We do not promote or recommend any treatment. We do not accept liability for any errors or omissions. Medical information, the law and government regulations change rapidly, so always consult your GP, pharmacist or other medical professional if you have any concerns or before starting any new treatment.
We welcome feedback on all our health information. If you would like to give feedback about this information, please email
If you don't have access to a printer and would like a printed version of this information sheet, or any other PKD Charity information, call the PKD Charity Helpline on 0300 111 1234 (weekdays, 9am-5pm) or email
The PKD Charity Helpline offers confidential support and information to anyone affected by PKD, including family, friends, carers, newly diagnosed or those who have lived with the condition for many years.

