Brain aneurysms
This information is for people with autosomal dominant polycystic kidney disease (ADPKD), their families and friends.
A brain aneurysm is a bulge in a blood vessel in the brain. Find out here about the risk of brain aneurysms for people with ADPKD. We explain screening, symptoms, diagnosis, and the treatment of brain aneurysms.
Finding out that you might be at higher risk of having a brain aneurysm can be scary. If reading this information causes you worry or you have any questions, please contact our helpline on 0300 111 1234 for support.
Contents
- Key Facts
- How common are brain aneurysms?
- Symptoms
- What problems can brain aneurysms cause?
- How are brain aneurysms diagnosed?
- What causes brain aneurysms in people with ADPKD?
- Reducing your risk of a brain aneurysm
- Treating brain aneurysms
- Fear of aneurysms
- How will I know if I get a bleed on the brain?
Key facts
- An aneurysm in the brain occurs when part of a blood vessel bulges out, like a small berry.
- Brain aneurysms are more common in people with autosomal dominant polycystic kidney disease (ADPKD) than in the general population.
- Brain aneurysms usually don’t cause problems.
- However, there is a small risk of them bursting and bleeding.
- People at higher risk of having a brain aneurysm can have check-ups.
- You can reduce your chance of having an aneurysm by following a healthy lifestyle.
- If you have a brain aneurysm at risk of bursting, you can have it treated to prevent this.
- Treatment for brain aneurysms usually works well.
- Finding out you might be at higher risk of having a brain aneurysm can be scary.
- If reading this fact sheet causes worry or you have questions, contact the helpline on 0300 111 1234 for support.
- If anxiety about brain aneurysms is affecting your life, talk to your GP or kidney specialist for help.
How common are brain aneurysms?
Brain aneurysms are also known as ‘intracranial aneurysms’.
Most people with ADPKD don’t have a brain aneurysm, but about 9 in every 100 people with ADPKD do.2,4 This compares with about 2 to 3 out of every 100 people in the general population.3
Brain aneurysms are more common in people with ADPKD from about age 30—40 years old onwards.2,4
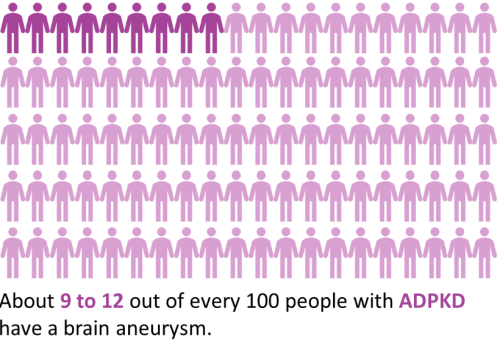
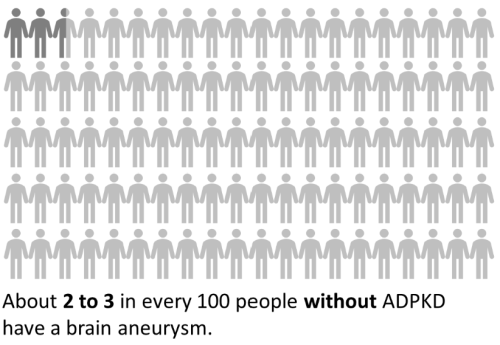
A diagram showing how common brain aneurysms are in people with ADPKD (about 9—12 in every 100 people) versus people without ADPKD (about 2—3 in every 100 people).
Symptoms
Most people with a brain aneurysm don’t have any symptoms and so will only know they have an aneurysm if they have a brain scan.4,5,9
Symptoms can occur if the aneurysm pushes on other parts of the brain or nerves.5,10 Symptoms can include:8
- vision problems, for example loss of vision or double vision
- pain above or around your eye
- numbness or weakness on one side of your face
- headaches
- seizures
See a doctor as soon as possible if you get any of these symptoms.
What problems can brain aneurysms cause?
Brain aneurysms usually don’t cause symptoms.5,9 Occasionally they can cause problems if they press on the brain or nerves (see above), or if they burst.
Brain aneurysms usually don’t burst.5,6 For example, in a study of 75 Americans with ADPKD and a brain aneurysm, the researchers followed people for an average of 9 years per person. None of the aneurysms burst in this period although some people had their aneurysm treated to reduce their risk.4
Put another way, people with a brain aneurysm have a less than 1 in 100 chance of it bursting each year.5,6 Some people have a lower or greater risk than others.
Although the risk of an aneurysm bursting is low, it’s a dangerous event if it occurs.
A burst aneurysm causes bleeding on the brain.5,7 This is a type of stroke called a ‘subarachnoid haemorrhage’.5,11 About 2 out of every 3 people survive this.5,7 Bleeding on the brain can also damage the brain, leading to disability.
If you have a brain aneurysm, the risk of it bursting will depend on:4,6
- how big it is
- where it is
- whether you have high blood pressure
- whether other people in your family have had a brain aneurysm or bleed on the brain
In people at higher risk, a procedure can prevent the aneurysm bursting. We explain this below (see How are brain aneurysms treated?).
How are brain aneurysms diagnosed?
Brain aneurysms usually don’t cause symptoms.5,9
People with a greater risk of developing a brain aneurysm can have check-up scans. This screening is not recommended routinely for everyone with ADPKD.7,9,10
You may be offered screening if:1,7,9,12
- You’ve had a brain aneurysm before.
- A family member has had a bleed on the brain or multiple people in your family have brain aneurysms.
- You have a job where falling unconscious could put others’ lives at risk.
- You’re having major surgery soon.
- You’re anxious about the risk of having a brain aneurysm and have discussed the pros and cons of screening with a counsellor.
Screening is usually done using an MRI (magnetic resonance imaging) scan.1,8 An MRI scanner is a large machine you lie in that produces a powerful magnetic field to see inside your body.
There is no set age to have screening — it depends on your risk.1 It’s usually done once every 5 or 10 years for people at increased risk. Some people at lower risk are offered screening once only.7,9,10
Scans can also be used if you have symptoms of an aneurysm.1,8 You’ll either have an MRI or a CT (computed tomography) scan.1,8 A CT scanner is a large machine you lie in that uses X-rays to see inside your body.
What causes brain aneurysms in people with ADPKD?
The gene faults that cause ADPKD might also alter the structure of blood vessels.10 These changes may make vessels in the brain weaker and more likely to bulge.
The risk of having a brain aneurysm is highest if you also have other risk factors:3,4,8
- smoking (doubles your risk)
- high blood pressure (doubles risk in people under 35 years)
- drinking a lot of alcohol
- having had a brain aneurysm or bleed on the brain before
- having a close relative (mother, father, brother, sister or child) who has had a bleed on the brain
- being female
- older age
- using cocaine
- being of Finnish or Japanese descent
Your risk of a brain aneurysm increases as you get older and as your ADPKD progresses.3,13
Most people with ADPKD have a fault in the PKD1 gene. Those who have a fault in the PKD2 gene have a lower risk of getting a brain aneurysm than those with a PKD1 fault.3
Reducing your risk of a brain aneurysm

A picture of a middle-aged man on an exercise bike.
You can reduce your chance of having a brain aneurysm by following a healthy lifestyle: 1,7,8
- Exercise regularly, eat a healthy diet, and stay a healthy weight to reduce your risk of high blood pressure.
- If you have high blood pressure or other cardiovascular problems, follow your doctor’s (GP’s) advice about diet, exercise, and medications.
- Give up smoking.
- If you drink alcohol, drink in moderation (a maximum of 14 units per week).
The steps above can also reduce the risk of a brain aneurysm bursting.
A brain aneurysm should not stop you having sex or exercising. If you’re unsure which types of exercise are suitable, ask your doctor for advice.
Women at increased risk of having a brain aneurysm (or who have been diagnosed with one already) should raise this with their doctor before using hormone-based contraception (for example, ‘the pill’, intrauterine device, implant or patch).
Treating brain aneurysms
A kidney specialist (nephrologist), brain surgeon (neurosurgeon), and specialist in using brain scans during treatment (interventional neuroradiologist) may be involved in your care.
The chance of an aneurysm bursting depends on its size and location in the brain. 4,6 If your aneurysm is low risk, you’ll be offered regular scans to check it rather than immediate treatment. 7,10 This is called ‘watchful waiting’ or ‘active observation’.
If the aneurysm becomes larger, your doctor might recommend treatment.
Treatment for an aneurysm involves a procedure to stop blood flowing into the bulge in the vessel. This is only recommended for people at higher risk of their aneurysm bursting. The two main procedures are: 1,5
- Coiling. Your surgeon will put a coil of very fine wire into the aneurysm. This causes the blood inside it to clot. This is called ‘endovascular coiling’ or ‘endovascular embolization’. The coil is inserted by feeding a very fine tube through a blood vessel in your leg up to your brain. Click here for a video showing how coiling works.
- Clipping. Your surgeon will put a metal clip on the artery to hold the aneurysm closed. This is called neurosurgical clipping. This is done as an operation through your head.
For 9 out of 10 people, these treatments work well to prevent complications. 5
Some aneurysms are more suited to coiling and others to clipping. There are pros and cons to each treatment type, but the overall risks are similar. There is a small risk of stroke with either procedure.14
If your treatment team thinks your aneurysm has a high risk of bursting, they’ll talk you through the risks and benefits of treating it. You’ll be able to choose whether to go ahead.
Fear of aneurysms
Some of our supporters say the risk of a brain aneurysm scares them. People who have had an aneurysm burst can also have long-term emotional problems such as depression. 15
If anxiety about brain aneurysms is affecting your life, talk to your GP or kidney specialist. They may be able to refer you to a counsellor or other healthcare professional who can help. They’ll also be able to recommend what you can do to reduce your risk.
You may also find it helpful to talk to other people with ADPKD. See our web page on PKD online support, or call our support line on 0300 111 1234 for ways to connect with others.
How will I know if I get a bleed on the brain?
Some of our supporters say the risk of a brain aneurysm scares them. People who have had an aneurysm burst can also have long-term emotional problems such as depression. 15
Symptoms of a burst aneurysm causing bleeding on the brain are usually very sudden. They include: 8
- an instant, excruciating headache. This would be unlike any headache you’ve had before. It might last a few seconds or may continue.
- feeling or being sick
- a stiff neck or neck pain
- sensitivity to light
- blurred or double vision
- sudden confusion
- loss of consciousness
- fits (seizures)
- weakness of an arm, leg, or side of your body.
You may also find it helpful to talk to other people with ADPKD. See our web page on PKD online support, or call our support line on 0300 111 1234 for ways to connect with others.
Telephone 999 for an ambulance immediately if you or someone else has these symptoms.
In most cases, a sudden, excruciating headache is not caused by a bleed on the brain, but it’s best to check. 16
More from the PKD Charity
More Information from the PKD Charity
- The UK Brain and Spine Foundation (0808 808 1000) has information on subarachnoid haemorrhage and the treatment of brain aneurysms.
- RadiologyInfo.org has detailed information on MRI and CT scans.
- The Stroke Association (0300 3300 740) is a UK charity providing information and support for people who have had a stroke, including a burst aneurysm.
Headway (0808 800 2244) is a UK charity providing information and support for people with a brain injury, including injuries that can occur as a result of a burst aneurysm.
References
- Stoneley C. Patient information. Brain aneurysms (including screening for familial aneurysms). January 2021.
- Irazabal MV, Huston J, Kubly V, et al. Extended follow-up of unruptured intracranial aneurysms detected by presymptomatic screening in patients with autosomal dominant polycystic kidney disease. Clinical Journal of the American Society for Nephrology. 2011;6(6):1274-85.
- Lefèvre S, Audrézet M-P, Halimi J-M, et al. Diagnosis and risk factors for intracranial aneurysms in autosomal polycystic kidney disease: a cross-sectional study from the Genkyst cohort. Nephrol Dial Transplant. 2022;gfac027.
- Sanchis IM, Shukoor S, Irazabal, et al. Presymptomatic screening for intracranial aneurysms in patients with autosomal dominant polycystic kidney disease. Clinical Journal of the American Society for Nephrology. 2019;14(8):1151-1160.
- Williams LN, Brown RD. Management of unruptured intracranial aneurysms. Neurology Clinical Practice. 2013;3:99–108.
- Greving JP, Wermer MJ, Brown RD Jr, et al. Development of the PHASES score for prediction of risk of rupture of intra-cranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurology. 2014;13(1):59-66.
- KDIGO. Autosomal dominant polycystic kidney disease (ADPKD): Report from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney International. 2015;88:17-27.
- NHS. Brain aneurysms. Updated 11 April 2022.
- Harris PC, Torres VE. Polycystic kidney disease, autosomal dominant. GeneReviews® [Internet]. Last Updated 11 June 2015.
- Torres VE. Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369:1287–1301.
- Srivastava A, Patel N. Autosomal Dominant Polycystic Kidney Disease. American Family Physician. 2014;90:303-307.
- Lee VW, Dexter MAJ, Mai J, et al. KHA-CARI autosomal dominant polycystic kidney disease guideline: management of intracranial aneurysms. Seminars in Nephrology. 2015;35:612–617.
- Kuo IY, Chapman A. Intracranial aneurysms in ADPKD. How far have we come?. Clinical Journal of the American Society of Nephrology. 2019;14:1119–1121.
- Algra AM, Lindgren A, Vergouwen MDI, et al. Procedural clinical complications, case-fatality risks, and risk factors in endovascular and neurosurgical treatment of unruptured intracranial aneurysms: a systematic review and meta-analysis. Journal of the American Medical Association Neurology. 2019;76(3):282-293.
- NHS. Subarachnoid haemorrhage. Updated 2 December 2021.
- Patient.info. Subarachnoid Haemorrhage. Updated 20 November 2019.
Authors and contributors
Written by Hannah Bridges, PhD, Independent Medical Writer, HB Health Comms Ltd. Expert review by Professor Diederik Butlers, Neurosurgeon, University Hospital Southampton NHS Foundation Trust, and Mr Samuel Hall, Neurosurgery Registrar, University Hospital Southampton NHS Foundation Trust.
With thanks to all those affected by ADPKD who contributed to this publication.
© November 2024 (v2.0). Due for medical review November 2027.
IS Ref No: ADPKD.BA.V2.0
Disclaimer: This information is primarily for people in the UK. We have made every effort to ensure that the information we provide is correct and up to date. However, it is not a substitute for professional medical advice or a medical examination. We do not promote or recommend any treatment. We do not accept liability for any errors or omissions. Medical information, the law and government regulations change rapidly, so always consult your GP, pharmacist or other medical professional if you have any concerns or before starting any new treatment.
We welcome feedback on all our health information. If you would like to give feedback about this information, please email .
If you don't have access to a printer and would like a printed version of this information sheet, or any other PKD Charity information, call the PKD Charity Helpline on 0300 111 1234 (weekdays, 9am-5pm) or email .
The PKD Charity Helpline offers confidential support and information to anyone affected by PKD, including family, friends, carers, newly diagnosed or those who have lived with the condition for many years.

