Polycystic Kidney Disease (PKD)
Understanding PKD
Understanding polycystic kidney disease (PKD) and its types, symptoms, diagnosis, treatment, and lifestyle considerations is important for managing this chronic condition. Since 2000, our mission has been to raise awareness of PKD, support affected families and fund research for better treatments, care and a potential cure.
This page will assess important information related to PKD, from how common it is to how it affects the lives of those who have it; the more people understand this disease, the more work we can do to support and manage it.
What is Polycystic Kidney Disease (PKD)?
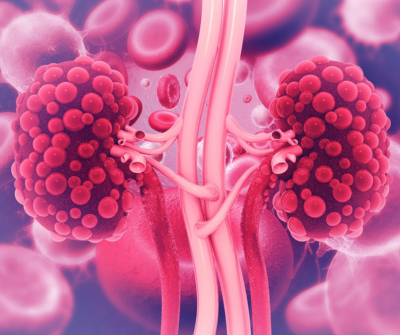
PKD is a genetic disorder that affects people of all ages, races and ethnicities and occurs equally in males and females. PKD primarily affects the kidneys, causing the growth of numerous fluid-filled cysts. These cysts can significantly enlarge the kidneys and impair their function over time, leading to serious health complications such as chronic kidney disease (CKD) and end-stage renal disease (ESRD). PKD is usually inherited from an affected parent in ADPKD, or from carrier parents in ARPKD. It can also result from a spontaneous genetic mutation.
There are two main types of PKD: Autosomal Dominant Polycystic Kidney Disease (ADPKD), which typically manifests in adulthood and is caused by a mutation in either the PKD1 or PKD2 genes, and Autosomal Recessive Polycystic Kidney Disease (ARPKD), a rarer form that presents in babies and young children due to mutations in the PKD1 gene. It's estimated up to 1 in every 1000 to 2500 people in the UK has ADPKD, and roughly 1 in 20,000 babies are born with ARPKD.

What Causes PKD?
PKD is caused by genetic flaws which vary depending on which type the person has.
ADPKD
For ADPKD, a person needs only one copy of a mutated PKD1 Or PKD2 gene from an affected parent to develop the disease, known as an “Autosomal Dominant” inheritance pattern. If one parent has a faulty PKD1 or PKD2 gene, there is a 50% chance that each child they have will inherit the condition.
ARPKD
ARPKD follows a different inheritance pattern, known as “Autosomal Recessive”. A person must inherit two copies of the mutated gene, one from each parent, to develop the disease. If both parents are carriers of the ARPKD gene mutation, there is a 25% chance that each child they have will inherit the condition. Carriers of the disease do not actually have the disease themselves.
Spontaneous Mutations
In rare cases, PKD can result from spontaneous mutations in the PKD1 or PKD2 genes, meaning the disease can occur even without a family history of PKD. This is more common in ADPKD than in ARPKD.
What Are the Symptoms of PKD?
Many symptoms of PKD are shared with other illnesses and diseases, so if you do not have a family history of this disease, they are unlikely to be related. Usual symptoms of PKD include:
-
High blood pressure (hypertension)
-
Pain in the back or sides
-
Blood in the urine (hematuria)
-
Frequent kidney infections
-
Headaches
-
Urinary tract infections (UTIs)
-
Kidney stones
-
Increased size of your abdomen (due to enlarged kidneys)
-
Decreased kidney function, potentially leading to chronic kidney disease (CKD) and end-stage renal disease (ESRD)
If you have any symptoms, alongside a first-degree relative with PKD (parent, child or sibling), it is important to speak to a doctor and schedule a screening appointment. Some people have more obvious symptoms than others, and it is not uncommon to have the disease for years without knowing you have it.

How is PKD Diagnosed?
PKD is usually diagnosed through the following three ways:
Imaging Tests
-
Ultrasound: The most common initial test used to detect cysts in the kidneys, ultrasounds are non-invasive and widely available in hospitals.
-
CT Scan: This machine provides more detailed images than an ultrasound, which is helpful in identifying smaller cysts and complications.
-
MRI: MRI scanners offer high-resolution images, beneficial for assessing the number and size of cysts and monitoring disease progression over time.
Genetic Testing
-
Blood Tests: This form of testing identifies mutations in the PKD1 or PKD2 genes. Genetic testing is particularly useful for early diagnosis in individuals with a family history of PKD or for those where imaging results are inconclusive.
-
Family History Analysis: Taking a detailed family history can help identify patterns of inheritance and assess risk, particularly in cases of ADPKD.
Laboratory Tests
-
Blood Tests: Blood tests are also used to measure kidney function by checking levels of creatinine and blood urea nitrogen (BUN).
-
Urine Tests: This form of testing checks for blood or protein in the urine, which can indicate signs of kidney damage.

How is PKD Monitored?
If you’re diagnosed with PKD, frequent monitoring will occur to measure and manage the disease. This is done in the following ways:
-
Regular Check-Ups: Frequent visits to a nephrologist (kidney specialist) will be scheduled to monitor kidney function and disease progression. Your blood pressure will also be checked and monitored since high blood pressure is a common complication of the disease.
-
Periodic Imaging: Regular ultrasounds, CT scans, or MRIs will be organised to monitor the size and number of kidney cysts and detect any new complications.
-
Blood and Urine Tests: Routine blood tests will be used to monitor kidney function, and urine tests will be scheduled to check for signs of infection or kidney damage.
What Problems Does PKD Cause?
Several health complications can arise if you have PKD. These include:
Chronic Kidney Disease (CKD)
Over time, the growing cysts caused by PKD can damage kidney tissue, leading to decreased kidney function. This can cause symptoms such as fatigue, changes in urination, and swelling in the ankles and legs.
End-Stage Renal Disease
The kidney damage caused by PKD can decline kidney function to the stage where a kidney transplant or dialysis is necessary.
High Blood Pressure (Hypertension)
High blood pressure is common for those with PKD due to cysts affecting blood flow and kidney function. This creates an increased risk of heart disease and strokes.
Kidney Stones
An altered kidney structure and function can lead to the formation of kidney stones. This can bring severe pain, blood in the urine and the presence of urinary tract infections (UTIs).
Kidney Infections
This disease can cause cysts to become infected, leading to more frequent UTIs. Symptoms associated with this include a general fever, back pain and an increased need to urinate.
Other Complications
There are rarer complications attached to PKD which some people may experience. This disease brings an increased risk of aneurysms since it can cause a swollen small artery in the brain. Brain aneurysms may be more likely in people with ADPKD because the gene alterations that cause ADPKD might also affect blood vessels.
People with PKD and kidney failure may develop diverticular disease and diverticulitis, where a formation of small pouches in the colon wall becomes inflamed or infected, bringing abdominal pain and changes in bowel habits.
Those who have mutated PKD1 genes may experience mitral valve prolapse. Although this is often asymptomatic, it can often cause palpitations or fatigue in more severe cases.

How is PKD Treated?
While there is currently no cure for PKD, treatments focus on managing symptoms and slowing the progression of the disease. Medications are often used to help manage pain, treat associated infections and lower blood pressure, and are effective for most people experiencing the disease. However, some people may need surgical procedures to drain and treat larger cysts on the kidneys to prevent further damage.
If your kidneys fail, treatment will be needed to restore some function, known as “kidney replacement therapy”. The most common form of this is a kidney transplant, received by a donor. Since you only need one kidney to live, kidney transplants are more accessible than other organ transplants, and living donors can give a kidney. However, most kidney donations still come from deceased donors.
Where a transplant is not possible either due to ineligibility or a shortage of organs, patients are instead put on dialysis, where a machine replicates some of the kidney’s functions. There are two types of dialysis; Hemodialysis and Peritoneal dialysis.
Further research into PKD has led to the approval of a treatment for adults which slows the rate at which your kidneys are enlarged by cysts, as well as slowing the speed at which your kidney function declines. This treatment, known as Tolvaptan, is taken orally (in tablet form) but is generally only available for adults who have PKD and chronic kidney disease stage 2 or 3, and show evidence that the disease is progressing quickly.

How Does PKD Affect Someone’s Daily Life?
This disease can significantly impact a person's daily life in various ways, depending on the severity of the disease and the presence of complications. Here are some key aspects of how PKD can affect daily living:
Emotional Impact
Stress, anxiety and depression can be common emotional symptoms in those who are dealing with PKD. Dealing with a long-term, progressive illness can lead to feelings of helplessness and depression, and worries about the progression of the disease and potential kidney failure can create anxiety and stress. If you’re experiencing these symptoms, it is important to reach out.
Insurance
The cost of your insurance could be affected if you have a family history of PKD, or if you’re diagnosed with it. If either of these outcomes is the case, it is important to disclose this information with your insurance provider, otherwise your insurance could be invalidated.
Dietary Requirements
Since the kidneys are affected by PKD, fluid intake could be balanced to avoid dehydration and kidney strain. People living with this disease require a low-sodium diet, so careful planning and preparation are needed to avoid high-salt foods.
Employment
Flexible work arrangements may be needed to accommodate regular medical appointments and variable energy levels. Fatigue and pain can decrease work efficiency and could lead to an increase in absences.
Social Participation
Pain, fatigue, and dietary restrictions can limit social interactions and participation in events. To deal with this, a strong support network of family and friends is crucial; otherwise, a feeling of social isolation can occur due to the chronic nature of the disease.
Driving
For those with PKD who drive a car or motorbike, you do not need to inform the DVLA. However, for those who drive a coach, bus or lorry, or if you have a brain aneurysm, the DVLA need to be informed. Consult with your doctor for any other queries regarding driving whilst managing this disease, such as how safe you are to drive following a dialysis session.
What Should You Do to Help Your Kidneys?
There are several tweaks that you should consider to your daily lifestyle to protect your kidneys and keep them as healthy as possible, such as:
Regular Exercise
It is important to regularly exercise to manage your blood pressure and body weight. Dealing with PKD can bring fatigue and pain, so consider how you can adapt forms of exercise to best manage this.
Healthy Eating
It is important to have a balanced diet, especially for those with PKD. This includes a low-salt diet to help manage blood pressure and reduce the rate your kidneys decline. Being overweight may increase your risk of higher blood pressure or cardiovascular problems, and may also lead to a faster decline of your kidneys.
Avoid Smoking
Smoking contributes to bad general health, leading to other negative health implications. However, it also can increase the speed that your PKD progresses, and cause further damage to your kidneys, leading to kidney failure.
Control Your Blood Pressure
If you have high blood pressure, it’s crucial to keep it under control; unmanaged high blood pressure raises the risk of a heart attack or a brain bleed (intracranial haemorrhage). Blood pressure can be treated with lifestyle changes and certain medications.
Avoid NSAIDs
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are frequently used to alleviate pain and inflammation. However, prolonged or repeated use can cause kidney damage, so it is important to consult with your doctor to find safer alternatives to use instead.

Finding Support If You’re Living With PKD
Our charity has many different ways in which you can get the support you need if you’re dealing with ADPKD or ARPKD. These include:

Looking to Fundraise?
We wouldn’t be able to continually support people affected by PKD without our wonderful fundraisers. By getting involved, you’re making a huge difference to the PKD community, spreading awareness and helping to fund further research. If you need fundraising inspiration, check out our A-Z of fundraising ideas, or get in touch with us - we’d love to hear from you!
Useful Links
-
Kidney Research UK has information on the latest research into all forms of kidney disease.
-
Kidney Care UK provides grants and other financial support to all kidney patients.
-
The National Kidney Federation has local kidney patient groups associated with kidney units in hospitals around the UK.
-
The NHS website has health information on a wide range of topics.
-
RaDaR Registry is a UK-wide registry of adults and children with rare kidney diseases including ADPKD. If you’re interested in joining the registry, please ask your kidney doctor for more information, or visit the website.
